Understanding Blood Types
Blood is an essential component of human physiology, integral to sustaining life. It functions as the body’s transport system, delivering indispensable nutrients and oxygen to cells while removing carbon dioxide and other waste products. In medical treatments, particularly during surgeries and after injuries, the compatibility of blood types becomes crucial to ensure safe blood transfusions.
The classification of blood types is rooted in the presence or absence of specific antibodies and antigens on the surface of red blood cells. These biological markers determine how the body reacts to foreign substances. The primary blood grouping is based on these markers, forming the four major blood groups: A, B, AB, and O. These groups are further categorized by the presence or absence of the Rh factor, leading to the emergence of eight possible blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-. The Rh factor, a protein found on the surface of red blood cells, provides additional specificity, with its presence denoting a positive (+) blood type and its absence indicating a negative (-) blood type.
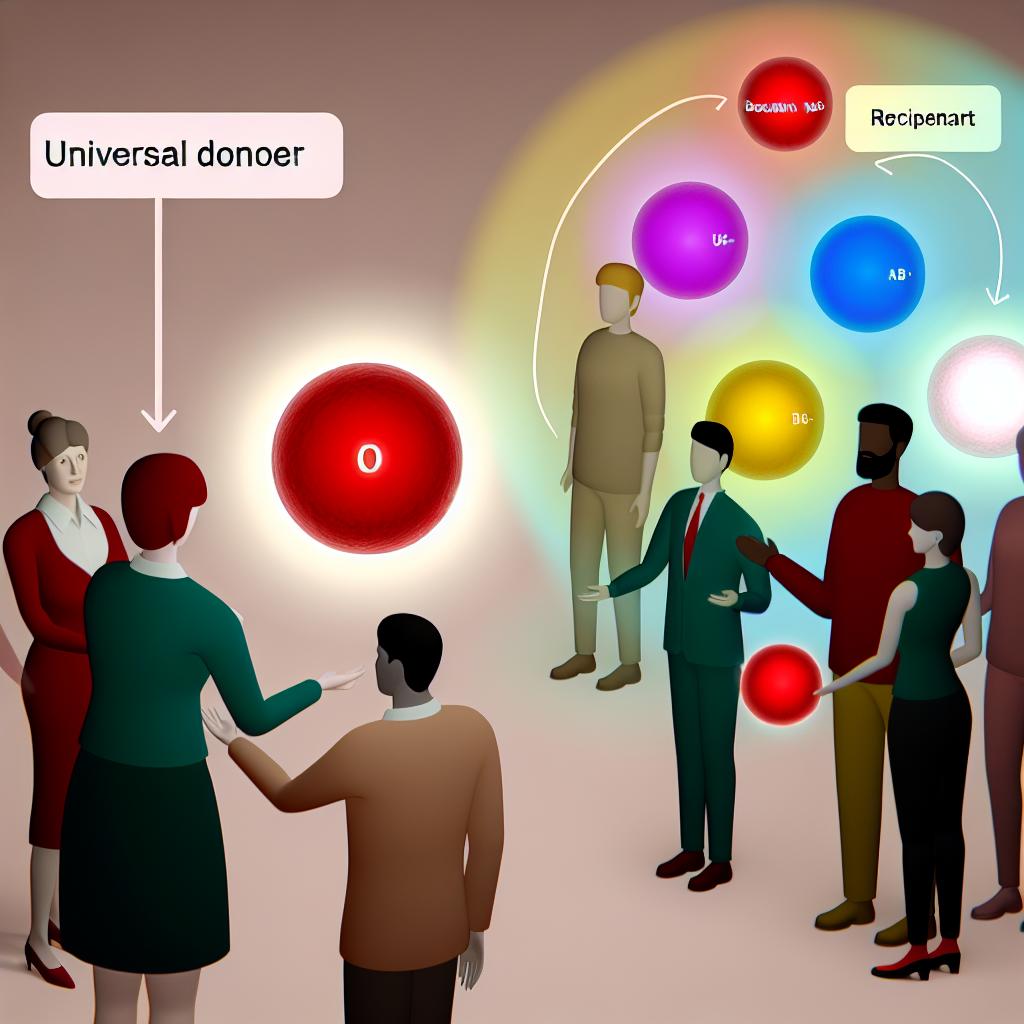
The Universal Blood Donor
The blood type O-negative (O-) holds a unique position due to its universal donor status. Individuals with O- blood can donate to any other blood type, as their red blood cells lack A and B antigens and the Rh factor, minimizing the risk of an immune response in recipients. During emergencies, where time is of the essence and blood type tests cannot be conducted swiftly, O- blood is a vital resource due to its universal acceptability.
However, despite this critical role, O- blood is relatively rare. It constitutes around 7% of the global population, which presents challenges in maintaining an adequate supply. The demand for O- blood often outpaces availability, necessitating regular donations from those few who possess this blood type. Its universal nature makes O- donations invaluable, not only in emergencies but also in circumstances where a patient’s blood type is unknown.
The Universal Recipient
Conversely, individuals with an AB-positive (AB+) blood type have the distinct advantage of being universal recipients. This means they can receive blood from any donor, regardless of the donor’s blood type. The presence of both A and B antigens and the Rh factor in AB+ individuals ensures that their bodies do not mount an immune reaction against transfused blood. This flexibility can be particularly advantageous in life-threatening situations where immediate blood transfusion is necessary, and the selection of compatible blood is constrained.
Despite their ability to receive diverse blood types, AB+ individuals face unique challenges concerning blood donation. Their blood is exclusively compatible with other AB+ recipients. Consequently, while they can widely receive blood, their ability to donate is substantially limited to a smaller recipient pool. This aspect underscores the heterogeneity of blood type compatibility – each type brings its own distinct benefits and limitations in the context of donation and reception.
The Importance of Blood Donation
Blood donation is a critical aspect of healthcare systems globally. Every donated unit of blood has the potential to save lives, as each donation can be separated into components to be used across various treatments. Applications of donated blood include surgeries, where blood loss necessitates transfusions, cancer treatments that often lead to compromised blood cell production, and chronic illness management where regular transfusions may be vital.
Moreover, the importance of blood donation extends to managing trauma care cases, where immediate blood transfusion can be a decisive factor in patient outcomes. The necessity for a robust, well-maintained blood supply becomes evident when considering these varied applications. Ensuring a steady inflow of donations is pivotal to overcoming shortages, which can have severe implications for healthcare delivery.
For those willing to be donors, numerous organizations and local blood banks provide resources and support. They outline pathways to donor eligibility and donation locations, often detailed on their web platforms. Engaging with these services facilitates the donation process and maximizes the potential impact of each contribution.
Conclusion
Grasping the dynamics of blood type compatibility, including the roles of universal donors and recipients, is fundamental to understanding the significance of blood in medical practices. Each blood type, whether O- or AB+, contributes uniquely to the challenges and solutions within the field of transfusion medicine. Routine blood donations are essential, serving as a linchpin in sustaining health systems and saving lives across the globe. Your participation as a blood donor can markedly influence resources available to hospitals and medical facilities, promoting better health outcomes for those in critical need.