Understanding Blood Type Compatibility
When it comes to medical science, particularly in the field of hematology and transfusion medicine, understanding blood type compatibility is of utmost importance. This essential knowledge guides healthcare professionals in safely administering blood transfusions and organ transplants. To comprehend how blood type compatibility works, one needs to delve into two primary systems that determine blood type: the ABO blood group system and the Rh factor. Understanding these systems not only aids medical professionals but also educates individuals about their own and others’ blood compatibility, potentially saving lives in emergency situations.
The ABO Blood Group System
The ABO blood group system is a classification scheme based on the presence or absence of specific antigens on the surface of red blood cells. These antigens are crucial, acting as molecular markers that trigger the body’s immune response. The definition of each blood group within the ABO system hinges on the combination of these antigens and the corresponding antibodies present in the plasma.
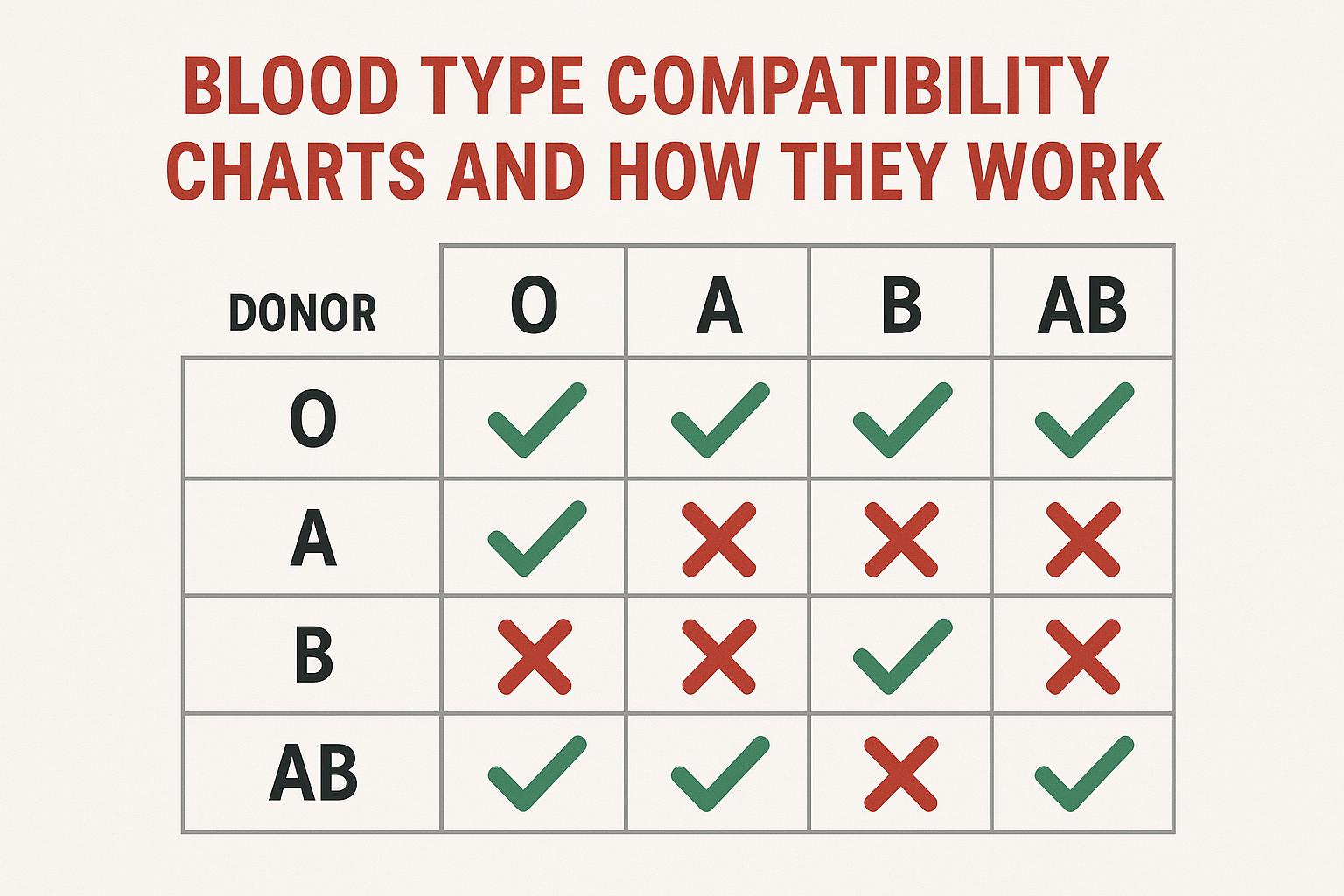
Type A blood, for example, features the A antigen on the cell surface and carries B antibodies in the plasma. This configuration means that individuals with Type A blood can accept Type A or Type O blood in transfusions, as the presence of B antibodies prohibits compatibility with Type B or AB blood.
In contrast, Type B blood contains the B antigen and A antibodies, allowing transfusion compatibility with Type B and Type O blood. The necessary avoidance of A antigens from Type A and AB blood is due to the immune response elicited by the presence of A antibodies.
Type AB blood is unique in that it possesses both A and B antigens yet lacks A and B antibodies. This absence allows individuals with Type AB blood to receive any ABO blood type, establishing them as universal recipients with respect to the ABO system.
Meanwhile, Type O blood is characterized by the complete absence of A and B antigens while carrying both types of antibodies within the plasma. Consequently, Type O individuals must only receive Type O blood to evade immune reactions. However, Type O’s lack of antigens grants them the distinction of being universal donors to all ABO blood types.
The Rh Factor
Beyond the ABO blood group system, the Rh factor, another antigen found on red blood cells, plays a vital role in blood type classification. The presence of the Rh antigen is denoted as Rh positive, whereas its absence is referred to as Rh negative. These qualifications are merged with the ABO blood types, resulting in a more comprehensive classification: A+, A-, B+, B-, AB+, AB-, O+, and O-.
Understanding Rh factor compatibility is crucial for safe medical practices. For instance, Rh-negative individuals should not receive Rh-positive blood due to the risk of an immune response. Such consideration becomes even more critical in contexts like pregnancy, where Rh incompatibility can present risks to both the mother and her unborn child.
Compatibility for Blood Transfusions
Blood transfusions require meticulous attention to both ABO and Rh factors to avert severe transfusion reactions. The fundamental guideline is to match, as closely as possible, the donor’s blood type with the recipient’s. However, certain universal donor and recipient characteristics simplify emergency donations.
Individuals with Type O- blood are esteemed as universal donors. The absence of A, B, and Rh antigens in their blood allows it to be safely transfused to anyone, regardless of the recipient’s specific ABO and Rh type.
In conjunction, individuals with Type AB+ blood find themselves as universal recipients amidst ABO and Rh factors. Their blood, containing both sets of antigens and Rh positivity, enables them to accept all other blood types without concern for ABO and Rh incompatibility.
Matching not only the blood type but the Rh factor is crucial in transfusion medicine. For example, a donor with A- blood can safely give blood to recipients with A+ or A- blood types. However, in reverse, A+ blood cannot be given to A- recipients due to the presence of the Rh antigen.
Applications and Importance
The comprehensive understanding of blood type compatibility stretches beyond the realm of transfusions. It is pivotal in organ transplantation procedures, emergency medical interventions, and even in everyday healthcare settings. When an organ transplant is in question, blood type matching is a routine consideration to minimize the risk of rejection. The donor and recipient must have compatible blood types to reduce the chances of immune-mediated complications.
Furthermore, blood type compatibility plays a significant role in pregnancy, particularly when an Rh-negative mother carries an Rh-positive fetus. This Rh incompatibility scenario necessitates medical supervision to prevent conditions such as hemolytic disease of the newborn. In some cases, administering medication can prevent an immunological response against the fetus’s blood.
The knowledge of one’s own blood type can be lifesaving in urgent medical situations, as well as when planning to donate blood. In a broader sense, community awareness about blood type compatibility can enhance preparedness and responsiveness to medical emergencies by potentially enabling self-assessment of blood transfusion compatibility.
Healthcare institutions, hospitals, and specialized organizations typically provide comprehensive resources on blood type compatibility to both medical professionals and the general public. These provide vital insights not only into the compatibility dynamics but also into procedural guidelines necessary for safe medical practices.
In conclusion, understanding blood type compatibility is a cornerstone of effective healthcare delivery. The intricacies of the ABO blood group system, paired with the Rh factor, form the foundation upon which safe blood transfusions and organ transplants are conducted. Familiarity with these principles can lead to more informed and safer clinical decisions, ultimately contributing to improved patient outcomes across a wide swath of medical applications.